Eye Care Articles
How to Choose the Best Eye Doctor in Western NY: Your Complete Guide
Choosing the right eye doctor is the first step in protecting your long-term eye health. Whether you’re booking your first eye exam, managing a...
Understanding Diabetic Eye Disease: Prevention and Management
Diabetes affects more than just your blood sugar. It can also have a serious impact on your vision. Over time, high blood glucose levels can damage...
A Patient’s Guide to Choosing the Right Eye Doctor: Opticians, Optometrists, and Ophthalmologists
Choosing the right eye doctor means better vision, improved eye health, and peace of mind. So, how do you decide who to trust with your eyes?...
Cataracts 101: Understanding Symptoms, Treatment, and Surgery in Buffalo, NY
Cataracts are one of the most common causes of vision loss, yet many people don’t recognize the early signs until their sight is significantly...
Advancements in Glaucoma Treatments: What Patients Need to Know
Glaucoma is one of the leading causes of irreversible vision loss worldwide, but advancements in treatments are offering hope for patients. With new...
Pediatric Eye Health: Ensuring Optimal Vision Development in Children
As a parent, you want to give your child every opportunity to succeed—and pediatric eye health plays a vital role in their development. From...
Open Your Eyes to the Threat of Glaucoma
Courtesy of Eye Care & Vision Associates (ECVA) The Cleveland Clinic says glaucoma is the second leading cause of blindness in...
Common Eye Health Questions
Our eyes are our windows to the world, yet with so much conflicting information out there, it's easy to feel uncertain about what truly affects...
Surgical Correction for Ptosis
Drooping eyelids, or ptosis, can significantly impact both appearance and vision, leading to a range of issues...
How Cataracts Can Lead to Vision Loss if Left Untreated
You might not realize it, but ignoring cataract symptoms can lead to blindness. Globally, cataracts are the leading cause of blindness, with 15.2...
How Drooping Eyelids Can Impact Your Vision
The impact of drooping eyelids is often far more significant than people expect. When the eyelids droop, it makes it difficult to see clearly or...
Can Surgery Correct Lazy Eye?
Lazy eye, or amblyopia, often goes unnoticed until it begins to affect daily activities. Imagine seeing the world through a lens that is always...
Recovering From Cataract Surgery: Buffalo Ophthalmologists’ Tips for a Smooth Recovery
If you live long enough, you will likely experience cataracts; they are a natural part of aging. The National Eye Institute says, “Cataracts are...
What Is the Best Macular Degeneration Treatment in WNY?
Macular degeneration is a severe eye condition that affects many people, especially as they age. One of the most effective treatments for macular...
How Sleep Impacts Your Vision
Quality sleep plays a vital role in maintaining overall health, including eye health. Sleep disorders such as sleep apnea and general sleep...
Trabeculectomy for Treating Glaucoma
Trabeculectomy is a surgical procedure designed to relieve intraocular pressure in patients with glaucoma, particularly when other treatments have...
Common Questions About Cataract Surgery Answered by Buffalo, NY Ophthalmologists
More than 6.1 million American cataract patients have successfully undergone surgery to remove them. This statistic marks the surgery as one of the...
The Causes of Secondary Glaucoma
Glaucoma is a group of eye conditions that damage the optic nerve – which is an essential part of vision – and is often linked to increased pressure...
Treating Retinal Tears and Detachments
Retinal tears and detachments are serious eye conditions that can lead to severe vision loss or blindness if not treated promptly. The retina – a...
Nutrition and Eye Health Tips from a Buffalo Ophthalmologist
You probably work out, eat well, and do your best to create a healthy lifestyle for your loved ones. But if you don't, you might also...
What Is the Safest Glaucoma Surgery?
Glaucoma is a group of eye conditions that damage the optic nerve and is often caused by abnormally high pressure in your eye. Left untreated,...
From Cataracts to LASIK: A Comprehensive Guide to Ophthalmological Procedures in Buffalo, NY
Buffalo, New York, boasts a vibrant community of ophthalmologists dedicated to providing top-tier eye care services. Eye Care & Vision...
When Is a Cornea Transplant Necessary? Understanding the Basics
Cornea transplants – a beacon of hope for individuals facing severe corneal damage or disease – stand as a testament to the incredible advances in...
How is a Laser Used in Laser Eye Surgery?
Laser eye surgery represents a groundbreaking leap in pursuing perfect vision, offering a sophisticated alternative to traditional eyewear and...
Optometrists vs. Ophthalmologists in Buffalo, NY: What is the Difference
Protecting your vision and the health of your eyes is essential. However, there are two types of professionals available: optometrists and...
Neurological Disease and the Eye
The intricate connection between the eye and the brain unfolds a compelling narrative in medical science, particularly in detecting and...
Safely Viewing the April 2024 Solar Eclipse in Buffalo, NY
As the April 2024 solar eclipse approaches, excitement builds in Buffalo, NY, where observers anticipate a breathtaking event. According to NASA,...
What Is Corneal Cross-linking?
In the world of ophthalmology, corneal cross-linking (CXL) stands out as a momentous advancement in treating corneal disorders. The procedure has...
Common Questions from Southern Ontario Residents Exploring Cataract Surgery in Buffalo
Cataracts can significantly impact your vision, affecting daily activities and overall quality of life. For Southern Ontario residents considering...
How is Lazy Eye Treated in Adults
Amblyopia, which is also colloquially referred to as lazy eye, is a condition that can impact people of all ages. While it's more common in...
Macular Degeneration Treatment Options in Western New York
Macular degeneration is an eye condition that leads to visual distortions and potentially permanent central vision loss. Often, it's a devastating...
The Benefits of Cataract Surgery in Buffalo for Southern Ontario Residents
When addressing the vision impairment caused by cataracts, residents of Southern Ontario are increasingly turning their gaze towards Buffalo, New...
Combined Cataract and Glaucoma Surgery: What to Expect
Both cataracts and glaucoma can rob a person of their vision, and the conditions can occur concurrently. For patients with cataracts and glaucoma,...
Am I a Candidate for iStent?
After a glaucoma diagnosis, finding a suitable treatment is crucial for preserving visual acuity. Glaucoma causes pressure to rise in the eye, and...
The Revolutionary iStent: A Minimally Invasive Solution for Glaucoma
Effective glaucoma treatment is critical for preserving a patient’s vision. Glaucoma is chronic and progressive, and without proper treatment, it...
Cataract Surgery in the Digital Age: How Technology is Revolutionizing Eye Care in WNY
Cataract surgery has come a long way from its humble beginnings, evolving into a sophisticated procedure that combines medical expertise with...
Exploring Minimally Invasive Glaucoma Surgery (MIGS)
Glaucoma is a chronic and progressive eye condition that’s also the leading cause of blindness in the world. Damage occurs as intraocular pressure...
The Evolution of LASIK: From PRK to Bladeless Femtosecond LASIK
Vision correction surgery began making headlines in the 1980s and 1990s. It generated excitement as people learned they may have a path to see...
Cataract Surgery in Orchard Park: What to Expect and How to Prepare
Cataracts are a common eye condition that can significantly impact your vision, making routine activities challenging. Fortunately, advancements in...
Beyond Eye Drops: The Advantages of Durysta Implant for Glaucoma Treatment
To put it simply, a glaucoma diagnosis is intimidating for many patients. Glaucoma is a leading cause of blindness. While there’s no cure for...
Big News: Orchard Park Vision Care Office Reopens with a Fresh Look!
We are delighted to announce the reopening of our Orchard Park eye care center, which officially took place on Monday, October 30th. This marks the...
Minimally Invasive Glaucoma Surgery in WNY is a Game-Changer in Treatment
About three million people each year in the U.S. live with the disease called glaucoma. One-half of these people don’t even realize they have the...
Diabetic Eye Disease and Vitreoretinal Surgery: Navigating Treatment Options
Diabetic eye disease like diabetic retinopathy can permanently alter a person’s vision, leading to vision loss or, in severe cases, blindness. With...
Durysta vs. Eye Drops: Choosing the Right Glaucoma Treatment for You
A glaucoma diagnosis is often scary, as glaucoma is one of the leading causes of blindness. While there is no cure for glaucoma, many treatment...
What to Expect After Glaucoma Surgery in WNY
There’s a reason why we call glaucoma the ‘silent thief of sight,’; 10% of patients who receive treatment still experience vision loss. Each year,...
The Role of Genetics in Eye Health: Understanding Inherited Eye Conditions
Some eye conditions are related to specific genetic markers. As a result, these eye conditions can be inherited. By understanding what conditions...
Postoperative Care Tips for Successful Cataract Surgery Recovery
Postoperative care plays a significant role in a successful cataract surgery recovery. By using the right approach, you can ensure the healing...
SLT Laser Surgery for Glaucoma: Redefining Care for Lasting Visual Health
Glaucoma, often called the "silent thief of sight," is a group of eye conditions that damage the optic nerve, leading to progressive vision loss and...
The Importance of Regular Eye Exams for the Whole Family
The start of the school year is on the horizon, so many households are taking the time to get ready for the upcoming academic year. One critical...
Common Age-Related Eye Problems
Vision plays a crucial role in everyone’s daily lives. But over time, age-related eye problems may arise, affecting a person’s ability to see...
Summer Eye Care Tips
It’s officially summer, a time of year when people spend more time outdoors enjoying the excellent weather. However, it’s also a season that comes...
Laser Cataract Surgery: Everything You Need to Know
If you live long enough, you may have laser-assisted cataract surgery. By age 80, 50% of Americans will likely have laser surgery for cataracts....
Myths About UV Protection and Your Eyes
Ultraviolet (UV) rays are harmful, including to your eyes. Since July is UV safety month, it’s the perfect time to consider how you can protect your...
What Is Eyelid Dermatitis?
Eyelid dermatitis is a form of contact dermatitis, a skin condition that occurs when you come into contact with a triggering substance, such as an...
Debunking Common Myths About Cataract Surgery
Myths persist about cataract surgery, even though it’s one of the most common and safest medical procedures in the United States. It makes sense,...
Does Health Insurance Cover Cataract Surgery?
Whether you recently learned that you have cataracts and want to prepare or are getting ready for cataract surgery, understanding your out-of-pocket...
The Impact of Cataract Surgery on Vision and Quality of Life
Half of Americans aged 80 or older have cataracts or had surgery to remove them. Cataract surgery is one of the most common medical procedures in...
Optometrist, Optician, or Ophthalmologist?
When you’re looking for a new eye care provider, you may notice that eye care providers can have several different titles. If you don’t know the...
Do Cataract Eye Drops Work?
The idea of a simple home treatment is incredibly appealing to patients with cataracts. As a result, many people look for information about cataract...
Cataract Surgery Recovery: Tips for a Speedy Healing Process
Cataract surgery is one of the most common surgical procedures in the world. In the U.S., 3.7 million people yearly have this life-changing surgical...
Should I Choose a Premium Cataract Lens?
Cataracts cause the eye’s lens to become cloudy, reducing visual acuity. During cataract surgery, the use of an intraocular lens (IOL) to replace...
Why Are My Eyes Burning?
Burning eyes are highly uncomfortable and may make it difficult to see clearly. The stinging sensation is highly distracting, and keeping the eyes...
Types of Retinal Detachment
Retinal detachments dramatically alter your vision and can lead to permanent changes that cost you your eyesight. While many people are at least...
How Can I Fix My Vision Problems?
If you’re experiencing shifts in your visual acuity, you may wonder if there are steps you can take to fix the vision problems you’re noticing....
Choosing a Premium Lens for Cataract Surgery: The Complete Guide
If you live long enough, nearly everyone will have cataracts, a medical condition that causes the deterioration of your vision. Cataracts currently...
What Causes Tunnel Vision?
Tunnel vision is a highly disruptive condition, making it difficult or impossible to see objects that aren’t positioned directly in front of you....
5 Reasons to Consider the Alcon PanOptix Lens for Cataract Surgery in Buffalo
As you age, you’ll likely have cataract surgery. Cataract surgery in Buffalo is a routine surgery to restore vision in older patients suffering from...
Questions to Ask Your Doctor About AMD
Receiving a diagnosis of age-related macular degeneration (AMD) is often startling and concerning, particularly if you aren't overly familiar with...
Ways to Take Better Care of Your Eyes in 2023
Caring for your eyes is an excellent way to help keep them healthy. Specific eye care habits can reduce your odds of developing specific conditions,...
Standard vs. Premium IOLs for Cataract Surgery: Is it Worth it to Upgrade?
Most people who live into their 70s will develop cataracts in one or both eyes. Cataracts cause a gradual dimming of vision and, if not corrected,...
What Are the First Signs of Glaucoma?
Glaucoma is an eye condition involving damage to the optic nerve, at times also including increased intraocular pressure. Over time, glaucoma...
What Is Thyroid Eye Disease?
hyroid eye disease (TED) is an autoimmune condition that impacts eye tissues. Typically, TED leads to inflammation, swelling, and damage to the...
Do I Have a Blocked Tear Duct or Stye?
For many patients, issues like bumps on your eye are immediately concerning. One common condition is a stye, which usually presents on the eyelid,...
How to Choose a Cataract Surgeon in Buffalo, NY
If you live long enough, the chances are high that you will end up with at least one cataract in your eyes. The American Academy of Ophthalmology...
ECVA Giving Back to the Community
Every year, ECVA gives back to the community by adopting a local veteran family for the holidays. This ECVA tradition started in 2015, and it’s...
Night Blindness and Trouble Seeing at Night
Many people struggle with seeing clearly at night. This is particularly true under specific conditions. For instance, glare created by headlights on...
Why Does Bright Light Bother My Eyes?
Many people’s eyes are bothered by bright light. A degree of photosensitivity, as a result, isn’t uncommon overall. However, the causes of...
Top Questions to Ask Your Doctor About Cataract Surgery
If you’re considering cataract surgery, you’re probably looking forward to the results but nervous about the process. That’s only natural, but it is...
When Is a Cornea Transplant Needed?
Cornea damage can impact patients in a variety of ways. It may lead to vision changes, preventing you from seeing clearly. Often, damage to the...
Why Am I Seeing Halos?
While light is critical for vision, it can also lead to some difficulties. One prime example is halos, rings of light around light sources. At...
Things Your Ophthalmologist Wishes You Knew
Maintaining proper eye health throughout the course of your life is essential. By doing so, you can potentially preserve your vision and get the...
Sunglasses After Cataract Surgery: A Guide
More than 10 million cataract surgeries are performed around the world each year. About four million of these are performed in the U.S. annually....
Why Back-to-School Eye Exams are Important
Back-to-school brings a flurry of activity to most family households. There are many tasks to accomplish before school starts and parents and their...
Are Dry Eyes Serious?
Dry eye is a relatively common condition where tear production doesn’t sufficiently keep the eye lubricated. The cause can vary, though it usually...
Questions to Ask When Considering Lasik
For many people who’ve spent time wearing contact lenses or glasses, Lasik may seem like an attractive alternative. Depending on various factors,...
Does a Retinal Detachment Heal on Its Own?
Retinal detachment is a severe medical condition that can cost you your vision. As a result, it should always be taken seriously, as quick action is...
Is a Dilated Eye Exam Necessary?
When you prepare for an eye appointment, you may discover that your eye care provider will dilate your eyes during the exam. Since that can lead to...
Can You Prevent Cataracts from Getting Worse?
Cataracts can have a dramatic impact on your vision, causing cloudiness that harms visual acuity and alters the visual field. Typically, cataracts...
Is Lasik Surgery Safe? What You Need to Know
Laser-assisted in situ keratomileusis – also known as LASIK – is a popular outpatient procedure for treating nearsightedness, farsightedness, and...
Cataract Surgery Success Rate
Cataract surgery is among the most common types of surgery. While it was once an inpatient procedure requiring general anesthesia, it can now be...
Can Cataracts Come Back After Surgery?
Cataracts, or an opacification or clouding of the eye’s lens, affect millions of people – it's one of the most common eye conditions in the world....
Why Is My Vision Getting Worse?
Many people know that vision changes can occur at any time. However, if your vision is declining year after year or suddenly takes a turn for the...
What Are the Early Signs of Glaucoma?
Glaucoma is an eye condition impacting the optic nerve. As intraocular pressure builds, damage to the optic nerve can occur, leading to permanent...
Three Common Vision Problems
When it comes to vision problems, refractive errors are the most common ones that people experience. With these, the shape of the eye or its ability...
How to Protect Vision Right Now
The prospect of vision loss is not typically a concern for most people until a decline in visual acuity becomes noticeable. Vision changes typically...
The Stages of Diabetic Retinopathy
When a person has diabetes, they’re at risk of a debilitating eye condition called diabetic retinopathy. Essentially, elevated blood sugar levels...
Cataract Treatment: Lasers vs. Traditional Cataract Surgery
Cataracts are some of the most common eye ailments and affect millions of people all over the globe, especially older folks. For many years,...
What is a Visual or Ocular Migraine
When people think of migraine headaches, physical discomfort or pain is usually the part that comes to mind first. However, migraines can also come...
Frequently Asked Questions About Your Eyes
Many people have questions about their eyes and vision, particularly regarding visual changes, discomfort, and safety. If you’re one of them, here...
Understanding Cataract Progression
Cataracts are an incredibly common eye condition, particularly as people get older. Often, the disease progresses slowly, giving those with...
AMD Awareness – Age-Related Macular Degeneration
February is Age-Related Macular Degeneration (AMD) Awareness Month, a time where we share information about this devastating condition. Along with...
Glaucoma Treatment and Management
During January, we recognize Glaucoma Awareness month by taking a close look at the eye condition. While we addressed what the condition is...
Early Glaucoma Detection
Glaucoma is a serious eye condition where fluid builds up in the eye, causing damage to the optic nerve. If not treated promptly, glaucoma can cause...
How Long Does It Take to Recover from Cataract Surgery?
When you’re preparing for cataract surgery, you may have questions about your recovery. While knowing that your vision quality will improve is part...
Taking Care of Dry Eyes in Winter
While the winter can be a magical time of year, it can also wreak havoc on your eyes. Falling temperatures, heater use, and other situations that...
The Different Types of Cataracts
Cataracts are a buildup of material in the eye that leads to lens clouding, altering a person’s vision. However, not all cataracts are the same. In...
5 Ways Diabetes Can Affect Your Vision and Health
If you have diabetes, you have a greater risk of developing certain eye diseases. By understanding what may occur, you can watch out for the signs...
What Are The Signs of Cataracts?
Most people are aware of cataracts, largely because it’s an incredibly common condition. Over 24 million adults over the age of 39 have...
Fall Eye Care Tips
For many people, fall is their favorite time of year. The heat of the summer starts to fade, and the leaves start changing, introducing warm,...
Why Are My Eyes So Watery?
At times, water eyes are simply an occasional annoyance. However, since excessive tearing (epiphora) can have various causes, watery eyes may also...
What Causes Eye Color to Change?
Changes in eye color can be as captivating as they are concerning. By understanding what can cause eye colors to change, you can determine if what...
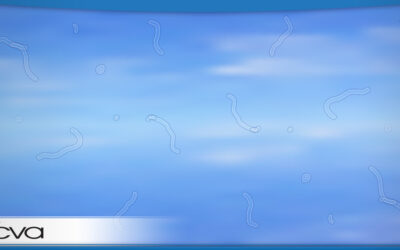
Spider Webs in Your Vision – What It Means, Why It Happens, and How Serious Is It?
Seeing spider webs across your vision can be concerning or at least momentarily distracting. However, some of the worry is often based on not...
Congenial (Pediatric) Cataracts – What It Is and How It’s Treated
When people think of cataracts, they typically associate the condition with older adults. However, cataracts can happen much earlier in life, and...
Congenial (Pediatric) Cataracts – What It Is and How It’s Treated
When people think of cataracts, they typically associate the condition with older adults. However, cataracts can happen much earlier in life, and...
August Is Children’s Eye Health and Safety Month
August is Children's Eye Health and Safety Month. It's a time where we focus on eye-related concerns that impact children and highlight the...
Common Eye Problems in Summer
During the summer months, most people focus on enjoying the warmer weather, planning vacations, and other fun events, not the eye problems they may...
Common Eye Problems in Summer
During the summer months, most people focus on enjoying the warmer weather, planning vacations, and other fun events, not the eye problems they may...
Pediatric Ptosis
Many parents aren’t familiar with all of the conditions that can impact their child’s eyes or vision. Pediatric ptosis, while common,...
Pediatric Ptosis
Many parents aren’t familiar with all of the conditions that can impact their child’s eyes or vision. Pediatric ptosis, while common,...
Summer Eye Care Tips
While taking care of your eyes is a year-round job, certain situations that could cause them harm are more common in the summer. If you want to keep...
Summer Eye Care Tips
While taking care of your eyes is a year-round job, certain situations that could cause them harm are more common in the summer. If you want to keep...
Diabetic Retinopathy: What It Is and Why an Annual Screening Is Essential
Diabetes can be incredibly difficult on the body. While most people understand its impact on blood sugar management, diabetes can also lead to a...
Diabetic Retinopathy: What It Is and Why an Annual Screening Is Essential
Diabetes can be incredibly difficult on the body. While most people understand its impact on blood sugar management, diabetes can also lead to a...
What to Expect as Our Eyes Age
Most people understand that aging impacts the human body. However, many people are caught off guard when it comes to how aging effects our...
Pediatric Conjunctivitis (Pink Eye)
Pediatric conjunctivitis – also known as pink eye – is incredibly common. Many children end up with the condition, though the exact cause can vary....
Does Dark Mode Reduce Eye Strain?
Many people believe that using the dark mode on their computer, smartphone, or tablet is better for their eyes. Usually, this is because dark mode...
Screen Use for Children, Is It Safe?
Many parents are aware that limiting their children's screen time is a good idea. However, most parents aren't entirely sure where they should draw...
When Is Eye Twitching Serious?
When you experience an eye twitch, it's common to be concerned. Not only is the sensation uncomfortable or bothersome, but it's hard to tell if the...
Some Hidden Signs of Vision Problems in Children
As a child grows, their eyes and vision can change. While parents may hope that their child would let them know if they are having trouble seeing,...
Broken Blood Vessel in the Eye – Is It Serious?
Spotting a broken blood vessel in the white section of your eye can be scary. Often, it stands out dramatically, which alone can be concerning....
When Should My Child Get an Eye Exam?
Most parents are diligent about caring for their child’s health. However, many overlook the importance of eye exams or aren’t fully aware of when...
What Are the Types of Glaucoma?
January is Glaucoma Awareness month, a time of year where we take a close look at the condition and focus on sharing information to help patients...
Strabismus (Crossed Eyes), Causes and Treatment
Strabismus – the technical term for crossed eyes – is a condition where a person's eyes don't point in the same direction simultaneously. Typically,...
A Big Thank You To Our Patients
Each year, ECVA hosts an annual basket raffle for the month of November to benefit a family in need at Christmas. The money raised gets matched by...
How to Tell If You Have a Scratched Cornea
The cornea is the thin, transparent outer layer of the eye that extends over the iris and pupil. Since it's on the surface of the eye, it can...
Caring for Your Eyes in Cold Weather
When the temperature drops, it’s essential to adjust your eye care routine. Dry heat, UV light, and outdoor activities can increase certain risks....
Caring for Your Eyes in Cold Weather
When the temperature drops, it’s essential to adjust your eye care routine. Dry heat, UV light, and outdoor activities can increase certain risks....
But My Vision Is Fine – Why Everyone Needs Eye Exams
Many people assume that if they can see clearly, their eyes must be healthy. As a result, they skip regular eye exams or only come in when they...
But My Vision Is Fine – Why Everyone Needs Eye Exams
Many people assume that if they can see clearly, their eyes must be healthy. As a result, they skip regular eye exams or only come in when they...
Types of Low Vision
There are numerous types of vision acuity changes, each with its own signs and symptoms. Some are simply differences in severity, while...
Do I Need Readers?
Over time, a person’s vision typically changes. Losing near vision is one such change, frequently impacting people as they reach their 40s and...
We Are Growing Our Team To Meet Western New York’s Growing Vision And Eye Care Needs
Eye Care & Vision Associates, LLP (ECVA) is pleased to announce the hiring of Dr. David Styn, O.D. A licensed optometrist, Styn will be...
A Deeper Look into Macular Degeneration
Previously, we’ve discussed the signs and symptoms of macular degeneration and treatment options available through your eye...
A Deeper Look into Macular Degeneration
Previously, we’ve discussed the signs and symptoms of macular degeneration and treatment options available through your eye...
What Is Your Eye Health IQ?
Many people have grown up knowing certain vision “facts.” They may have heard them from their parents as a child, passing the tidbit of vision along...
What Is Your Eye Health IQ?
Many people have grown up knowing certain vision “facts.” They may have heard them from their parents as a child, passing the tidbit of vision along...
What Is This Bump on My Eye!
Finding a bump near your eye is always startling. You may be wondering if it is dangerous or what you should do to handle it. How you...
Understanding Glaucoma
Glaucoma is an eye condition that can rob a person of their sight. It is the second-leading cause of blindness in the world, and...
UV Protection and Your Eyes
Most people know that ultraviolet (UV) light can be damaging thanks to its connection to sunburns and skin cancer. However, many people don’t...
When Are Eye Floaters Serious?
Eye floaters – those little spots, lines, or shapes that flow across your vision – aren't usually a big deal. There's a decent chance everyone will...
Cloudy Vision vs. Blurry Vision
Describing a vision issue is challenging for many patients. It’s hard to find the right words to express precisely what you’re experiencing. At...
Cloudy Vision vs. Blurry Vision
Describing a vision issue is challenging for many patients. It’s hard to find the right words to express precisely what you’re experiencing. At...
Recognize the Signs of Retinal Detachment
Retinal detachment is a serious condition that should always be treated as an emergency. Without quick intervention, permanent vision loss is...
How Blue Light Affects Our Eyes
Most people have heard that they should reduce their exposure to blue light. But it’s common to have questions, including why blue light could be...
Your Safety is Our Priority
Starting on Monday, May 18, 2020, all ECVA locations will be re-opening. Our goal is to provide high-quality eye care services to each and every one...