by ecvaeyeadminz | Jun 19, 2024 | Glaucoma
Trabeculectomy is a surgical procedure designed to relieve intraocular pressure in patients with glaucoma, particularly when other treatments have failed to achieve adequate control. This surgical approach can be crucial in preserving visual function by managing the...

by ecvaeyeadminz | Jun 4, 2024 | Glaucoma
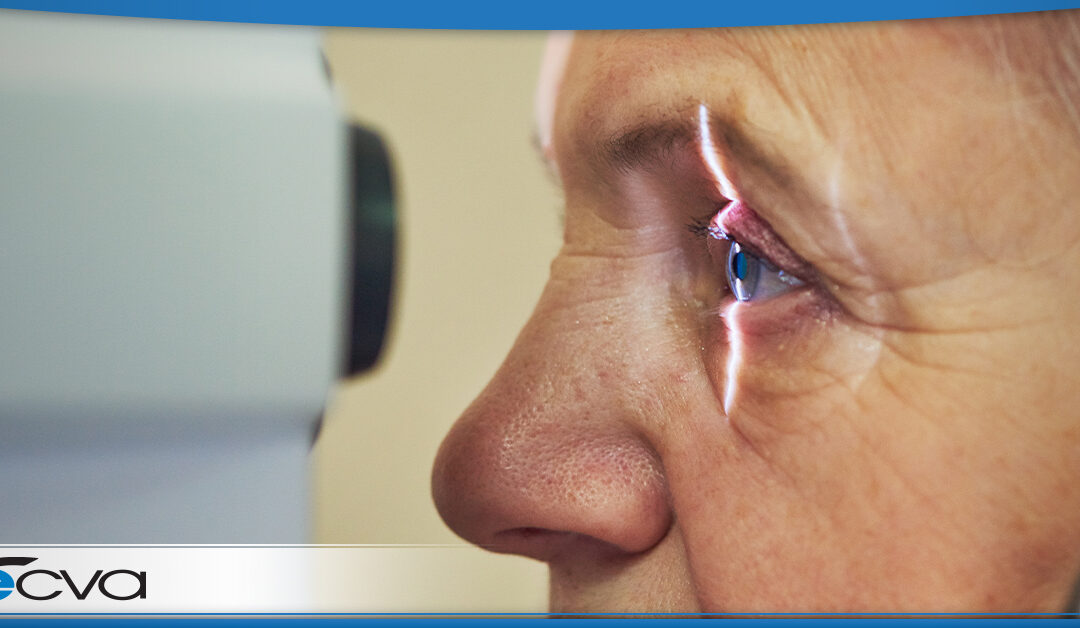
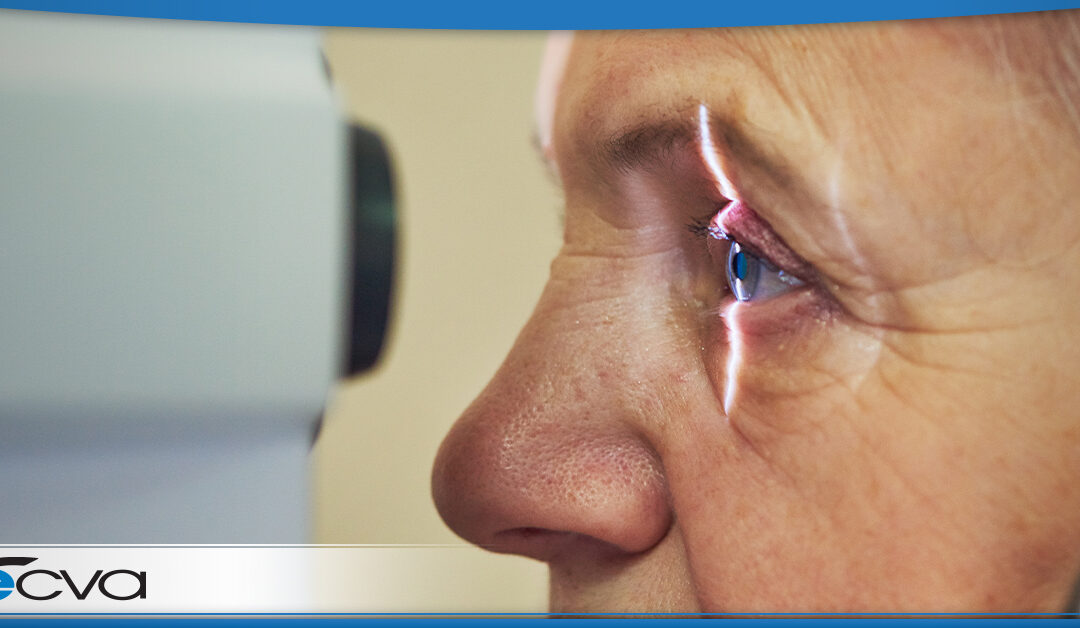
Glaucoma is a group of eye conditions that damage the optic nerve – which is an essential part of vision – and is often linked to increased pressure inside the eye. Secondary glaucoma, a type of this condition, arises as a complication of another medical issue or...

by ecvaeyeadminz | May 6, 2024 | Glaucoma
Glaucoma is a group of eye conditions that damage the optic nerve and is often caused by abnormally high pressure in your eye. Left untreated, glaucoma can lead to blindness. Fortunately, several surgical options are available for managing glaucoma, each with its own...

by preichert | Apr 29, 2024 | Cataracts, Glaucoma
Buffalo, New York, boasts a vibrant community of ophthalmologists dedicated to providing top-tier eye care services. Eye Care & Vision Associates (ECVA) is proud to be a member of this robust medical community. From addressing common conditions like cataracts to...
by ecvaeyeadminz | Jan 18, 2024 | Cataracts, Glaucoma
Both cataracts and glaucoma can rob a person of their vision, and the conditions can occur concurrently. For patients with cataracts and glaucoma, combined cataract and glaucoma surgery is often enticing. During the procedure, your eye care provider addresses both...

by ecvaeyeadminz | Jan 4, 2024 | Glaucoma
After a glaucoma diagnosis, finding a suitable treatment is crucial for preserving visual acuity. Glaucoma causes pressure to rise in the eye, and when that occurs, damage to the optic nerve can harm a person’s ability to see, potentially leading to permanent vision...