Courtesy of Eye Care & Vision Associates
Diabetes, a condition in which the body doesn’t easily produce or use insulin to control blood glucose levels, can also harm vision. Diabetic retinopathy, often called diabetic eye disease, is a serious vision problem where high blood sugar damages blood vessels in the retina, which may lead to permanent vision loss if not treated, according to medical professionals at Western New York’s Eye Care & Vision Associates (ECVA). The U.S. Centers for Disease Control and Prevention states that about 30.3 million adults in the United States have diabetes, and 90 percent of them have type 2 diabetes. People with type 2 diabetes are at higher risk for diabetic retinopathy and an additional eye condition called diabetic macular edema.
According to ECVA, diabetic retinopathy happens when high blood sugar levels damage the small blood vessels that supply the retina. In the advanced stages of diabetic retinopathy, the eye tries to grow new blood vessels, but these vessels develop improperly and can easily leak or bleed. The most common type of diabetic retinopathy is nonproliferative diabetic retinopathy (NPDR). With NPDR, new blood vessels do not form, but the walls of the blood vessels in the retina weaken. Tiny bulges form in the walls of smaller vessels, sometimes leaking fluid and blood into the retina. Sometimes, fluid can build up in the macula, the central part of the retina. This condition is called edema.
The most common signs of diabetic retinopathy include blurry vision, white or translucent visual floaters that appear and disappear, a faded appearance of colors, dull or dark areas in your field of vision, vision loss, and changes in your eyesight. The Mayo Clinic recommends that individuals see an ophthalmologist, especially one who specializes in retinal conditions, if they recognize any of these symptoms.
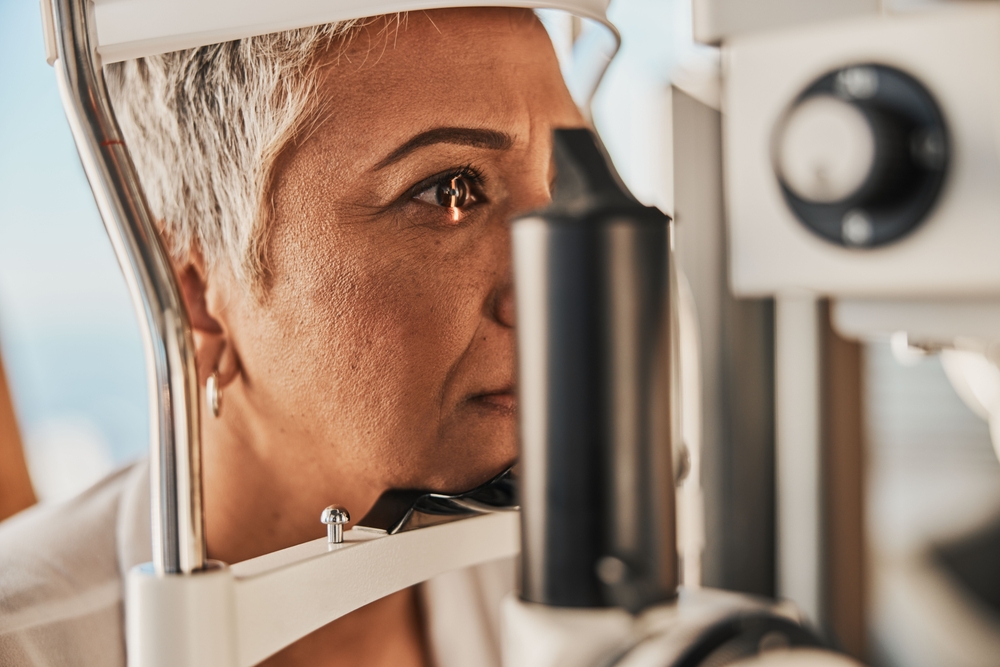
A dilated eye exam helps the eye doctor identify the cause of the symptoms and may also reveal a link to diabetes. In fact, vision exams are sometimes the first step in diagnosing diabetes. A dilated eye exam with an eye care professional is recommended annually, regardless of whether you have a history of eye health issues or a diabetes diagnosis. It is crucial to contact a medical professional immediately if vision suddenly changes or becomes blurry, hazy, or spotty, or if you see flashes of light.
Currently, there is no way to permanently reverse the effects of diabetic retinopathy, but there are options to manage the condition. During routine office visits, an ophthalmologist can inject medications directly into the eye to decrease retinal swelling and prevent the growth of abnormal blood vessels. However, the most effective treatment is to control blood sugar levels before symptoms worsen. Preventive care, such as regular exercise and a healthy diet, can lower a person’s risk of developing type 2 diabetes. Diabetic eye diseases can affect individuals with type 2 diabetes. Prevention, which involves regular visits to an eye care professional, is the best approach.
Learn more about Diabetic Retinopathy and watch a video at www.ecvaeyecare.com/diabetic-retinopathy. To schedule an appointment at ECVA, call 716-631-EYES (3937) or visit https://www.ecvaeyecare.com/contact-us//.